
国际生殖健康/计划生育 ›› 2022, Vol. 41 ›› Issue (1): 30-36.doi: 10.12280/gjszjk.20210379
收稿日期:2021-08-20
出版日期:2022-01-15
发布日期:2022-02-17
通讯作者:
王德娟
E-mail:wangdej@mail.sysu.edu.cn
GUO Qiang, QIU Jian-guang, WANG De-juan( )
)
Received:2021-08-20
Published:2022-01-15
Online:2022-02-17
Contact:
WANG De-juan
E-mail:wangdej@mail.sysu.edu.cn
摘要:
性发育异常(disorders of sex development,DSD)是一种表型和遗传高度异质的先天性疾病,其中46, XY性发育异常的病因和临床表现最为复杂多样,不及时治疗可能会给患者和家庭带来深远的影响。应综合患者病史、体格检查、实验室检查、影像学检查和分子遗传学检查进行诊断。目前DSD的治疗方式仍以手术治疗为主,性别心理决定和性别分配是46, XY DSD患者治疗中最关键的一环,应综合多学科团队、家属和(或)患儿本人的意见,结合患者性心理、性角色和性取向、性腺癌变风险、生育潜能、后续治疗和社会文化环境等因素进行,避免成年后要求改变性别的情况出现。性别分配后应尽早进行内外生殖器切除或修复手术并帮助患儿更好地适应分配的社会性别。目前国内外对于该病仍缺乏系统完善的诊疗指南,尤其是在46, XY DSD的病因诊断和外科手术的性别选择方面。
郭强, 邱剑光, 王德娟. 46, XY性发育异常的诊断和外科治疗研究进展[J]. 国际生殖健康/计划生育, 2022, 41(1): 30-36.
GUO Qiang, QIU Jian-guang, WANG De-juan. Diagnosis and Surgical Treatment of 46, XY Disorders of Sex Development[J]. Journal of International Reproductive Health/Family Planning, 2022, 41(1): 30-36.
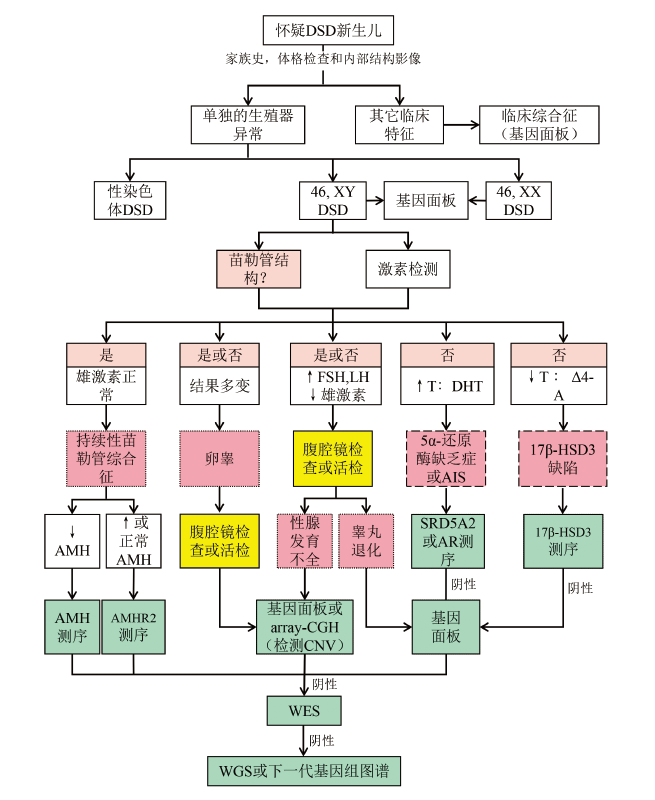
图1 怀疑46, XY DSD的新生儿诊断流程[19] 注:粉红色框代表类固醇生成途径(虚线框)或性腺发育(点状框)中的变异导致的疑似诊断。当激素检测或苗勒管检测难以评估时,可能需要使用腹腔镜检查和活检(黄色框)或分子遗传学方法(绿色框)诊断。Δ4-A Δ4-雄烯二酮,AMH 抗苗勒管激素,array-CGH 微阵列比较基因组杂交,CNV 拷贝数变异,DHT 双氢睾酮,FSH 卵泡刺激素,LH 黄体生成激素,T 睾酮,AR 雄激素受体,17β-HSD3 17β-羟基类固醇脱氢酶3,WES 全外显子测序。
| [1] |
Lee PA, Houk CP, Ahmed SF, et al. Consensus statement on management of intersex disorders. International Consensus Conference on Intersex[J]. Pediatrics, 2006, 118(2):e488-e500. doi: 10.1542/peds.2006-0738.
doi: 10.1542/peds.2006-0738 URL |
| [2] |
Lee PA, Nordenström A, Houk CP, et al. Global Disorders of Sex Development Update since 2006: Perceptions, Approach and Care[J]. Horm Res Paediatr, 2016, 85(3):158-180. doi: 10.1159/000442975.
doi: 10.1159/000442975 URL |
| [3] |
Parivesh A, Barseghyan H, Délot E, et al. Translating genomics to the clinical diagnosis of disorders/differences of sex development[J]. Curr Top Dev Biol, 2019, 134:317-375. doi: 10.1016/bs.ctdb.2019.01.005.
doi: S0070-2153(19)30005-5 pmid: 30999980 |
| [4] |
García-Acero M, Moreno-Niño O, Suárez-Obando F, et al. Disorders of sex development: Genetic characterization of a patient cohort[J]. Mol Med Rep, 2020, 21(1):97-106. doi: 10.3892/mmr.2019.10819.
doi: 10.3892/mmr.2019.10819 pmid: 31746433 |
| [5] |
Xue M, Wang X, Li C, et al. Novel pathogenic mutations in disorders of sex development associated genes cause 46, XY complete gonadal dysgenesis[J]. Gene, 2019, 718:144072. doi: 10.1016/j.gene.2019.144072.
doi: 10.1016/j.gene.2019.144072 URL |
| [6] |
Mendonca BB, Batista RL, Domenice S, et al. Reprint of "Steroid 5α-reductase 2 deficiency"[J]. J Steroid Biochem Mol Biol, 2017, 165(Pt A):95-100. doi: 10.1016/j.jsbmb.2016.11.006.
doi: 10.1016/j.jsbmb.2016.11.006 URL |
| [7] |
Mao Y, Zhang K, Ma L, et al. Interaction between CYP1A1/CYP17A1 polymorphisms and parental risk factors in the risk of hypospadias in a Chinese population[J]. Sci Rep, 2019, 9(1):4123. doi: 10.1038/s41598-019-40755-8.
doi: 10.1038/s41598-019-40755-8 URL |
| [8] |
Picard JY, Josso N. Persistent Müllerian duct syndrome: an update[J]. Reprod Fertil Dev, 2019, 31(7):1240-1245. doi: 10.1071/RD17501.
doi: 10.1071/RD17501 URL |
| [9] |
Gulía C, Baldassarra S, Zangari A, et al. Androgen insensitivity syndrome[J]. Eur Rev Med Pharmacol Sci, 2018, 22(12):3873-3887. doi: 10.26355/eurrev_201806_15272.
doi: 10.26355/eurrev_201806_15272 |
| [10] |
Wisniewski AB, Batista RL, Costa E, et al. Management of 46,XY Differences/Disorders of Sex Development (DSD) Throughout Life[J]. Endocr Rev, 2019, 40(6):1547-1572. doi: 10.1210/er.2019-00049.
doi: 10.1210/er.2019-00049 pmid: 31365064 |
| [11] |
Zhao S, Pan L, Chen M, et al. Di-n-butyl phthalate induced autophagy of uroepithelial cells via inhibition of hedgehog signaling in newborn male hypospadias rats[J]. Toxicology, 2019, 428:152300. doi: 10.1016/j.tox.2019.152300.
doi: 10.1016/j.tox.2019.152300 URL |
| [12] |
Chen MJ, Karaviti LP, Roth DR, et al. Birth prevalence of hypospadias and hypospadias risk factors in newborn males in the United States from 1997 to 2012[J]. J Pediatr Urol, 2018, 14(5): 425.e1-e7. doi: 10.1016/j.jpurol.2018.08.024.
doi: 10.1016/j.jpurol.2018.08.024 |
| [13] |
Vora KA, Hanna CA, Neville KA, et al. Role of cross-campus multidisciplinary team meetings in decision-making for children and adolescents with differences of sex development/intersex[J]. J Paediatr Child Health, 2021, 57(9):1402-1407. doi: 10.1111/jpc.15474.
doi: 10.1111/jpc.15474 URL |
| [14] |
唐达星, 付君芬. 性别发育异常的新认识及外科选择[J]. 中华小儿外科杂志, 2016, 37(7):481-484. doi: 10.3760/cma.j.issn.0253-3006.2016.07.001.
doi: 10.3760/cma.j.issn.0253-3006.2016.07.001 |
| [15] |
Moshiri M, Chapman T, Fechner PY, et al. Evaluation and management of disorders of sex development: multidisciplinary approach to a complex diagnosis[J]. Radiographics, 2012, 32(6):1599-1618. doi: 10.1148/rg.326125507.
doi: 10.1148/rg.326125507 pmid: 23065160 |
| [16] |
Ahmed SF, Rodie M. Investigation and initial management of ambiguous genitalia[J]. Best Pract Res Clin Endocrinol Metab, 2010, 24(2):197-218. doi: 10.1016/j.beem.2009.12.001.
doi: 10.1016/j.beem.2009.12.001 URL |
| [17] |
El-Maouche D, Arlt W, Merke DP. Congenital adrenal hyperplasia[J]. Lancet, 2017, 390(10108):2194-2210. doi: 10.1016/S0140-6736(17)31431-9.
doi: S0140-6736(17)31431-9 pmid: 28576284 |
| [18] |
Cools M, Nordenström A, Robeva R, et al. Caring for individuals with a difference of sex development (DSD): a Consensus Statement[J]. Nat Rev Endocrinol, 2018, 14(7):415-429. doi: 10.1038/s41574-018-0010-8.
doi: 10.1038/s41574-018-0010-8 |
| [19] |
León NY, Reyes AP, Harley VR. A clinical algorithm to diagnose differences of sex development[J]. Lancet Diabetes Endocrinol, 2019, 7(7):560-574. doi: 10.1016/S2213-8587(18)30339-5.
doi: 10.1016/S2213-8587(18)30339-5 URL |
| [20] |
Délot EC, Vilain E. Towards improved genetic diagnosis of human differences of sex development[J]. Nat Rev Genet, 2021, 22(9):588-602. doi: 10.1038/s41576-021-00365-5.
doi: 10.1038/s41576-021-00365-5 URL |
| [21] |
范丽君. 5α-还原酶2缺乏症的诊疗新进展[J]. 国际儿科学杂志, 2018, 45(8):609-614. doi: 10.3760/cma.j.issn.1673-4408.2018. 08.009.
doi: 10.3760/cma.j.issn.1673-4408.2018. 08.009 |
| [22] |
Golombok S, Rust J. The Pre-School Activities Inventory: A Standardized Assessment of Gender Role in Children[J]. Psychol Assess, 1993, 5(2):131-136. doi: 10.1037/1040-3590.5.2.131.
doi: 10.1037/1040-3590.5.2.131 URL |
| [23] |
Boldizar JP. Assessing Sex Typing and Androgyny in Children: The Children′s Sex Role Inventory[J]. Dev Psychol, 1991, 27(3):505-515. doi: 10.1037/0012-1649.27.3.505.
doi: 10.1037/0012-1649.27.3.505 URL |
| [24] |
中华医学会小儿外科学分会泌尿外科学组. 性别发育异常中国专家诊疗共识[J]. 中华小儿外科杂志, 2019, 40(4):289-297. doi: 10.3760/cma.j.issn.0253-3006.2019.04.001.
doi: 10.3760/cma.j.issn.0253-3006.2019.04.001 |
| [25] |
Döhnert U, Wünsch L, Hiort O. Gonadectomy in Complete Androgen Insensitivity Syndrome: Why and When?[J]. Sex Dev, 2017, 11(4):171-174. doi: 10.1159/000478082.
doi: 10.1159/000478082 pmid: 28719904 |
| [26] |
杨屹, 殷晓鸣. 46,XY性别发育异常的性腺处理[J]. 临床小儿外科杂志, 2019, 18(3):167-171. doi: 10.3969/j.issn.1671-6353.2019.03.002.
doi: 10.3969/j.issn.1671-6353.2019.03.002 |
| [27] |
Mentessidou A, Gargano T, Lima M, et al. Laparoscopic versus open orchiopexy for palpable undescended testes: Systematic review and meta-analysis[J]. J Pediatr Surg,2021 Jul 6: S0022-3468(21)00481-4. doi: 10.1016/j.jpedsurg.2021.07.003.
doi: 10.1016/j.jpedsurg.2021.07.003 |
| [28] |
Clifford TG, Burg ML, Hu B, et al. Satisfaction With Testicular Prosjournal After Radical Orchiectomy[J]. Urology, 2018, 114:128-132. doi: 10.1016/j.urology.2017.12.006.
doi: S0090-4295(17)31315-8 pmid: 29288790 |
| [29] |
Kamal NS, Alayoubi A, Elfakhri KH, et al. Effects of formulation variables on the in vitro performance of testosterone transdermal gel[J]. Int J Pharm, 2020, 590:119951. doi: 10.1016/j.ijpharm.2020.119951.
doi: 10.1016/j.ijpharm.2020.119951 URL |
| [30] |
Mole RJ, Nash S, MacKenzie DN. Hypospadias[J]. BMJ, 2020, 369:m2070. doi: 10.1136/bmj.m2070.
doi: 10.1136/bmj.m2070 |
| [31] | Tekgül S, Dogan HS, Kocvara R, et al. EAU Guidelines on Paediatric Urology[M/OL]. Arnhem:European Association of Urology, 2017:21-26. http://uroweb.org/wp-content/uploads/21-Paediatric-Urology_2017_web.pdf. |
| [32] |
González R, Lingnau A, Ludwikowski BM. Results of Onlay Preputial Flap Urethroplasty for the Single-Stage Repair of Mid- and Proximal Hypospadias[J]. Front Pediatr, 2018, 6:19. doi: 10.3389/fped.2018.00019.
doi: 10.3389/fped.2018.00019 pmid: 29473028 |
| [33] |
Zhang Y, Shen Z, Zhou X, et al. Comparison of meatal-based flap (Mathieu) and tubularized incised-plate (TIP) urethroplasties for primary distal hypospadias: A systematic review and meta-analysis[J]. J Pediatr Surg, 2020, 55(12):2718-2727. doi: 10.1016/j.jpedsurg.2020.03.013.
doi: 10.1016/j.jpedsurg.2020.03.013 URL |
| [34] |
Acimi S, Abderrahmane N, Debbous L, et al. Koyanagi- Snow-Hayashi Urethroplasty in Severe Hypospadias Repair: Between Hope and Reality[J]. Urology, 2021, 152:129-135. doi: 10.1016/j.urology.2020.11.058.
doi: 10.1016/j.urology.2020.11.058 URL |
| [35] |
Wani SA, Baba AA, Mufti GN, et al. Bracka verses Byar′s two-stage repair in proximal hypospadias associated with severe chordee: a randomized comparative study[J]. Pediatr Surg Int, 2020, 36(8):965-970. doi: 10.1007/s00383-020-04697-x.
doi: 10.1007/s00383-020-04697-x URL |
| [36] |
Baumgarten L, Dabaja AA. Diagnosis and Management of Gynecomastia for Urologists[J]. Curr Urol Rep, 2018, 19(7):46. doi: 10.1007/s11934-018-0796-x.
doi: 10.1007/s11934-018-0796-x pmid: 29774423 |
| [37] |
Kudela G, Gawlik A, Koszutski T. Early Feminizing Genitoplasty in Girls with Congenital Adrenal Hyperplasia (CAH)-Analysis of Unified Surgical Management[J]. Int J Environ Res Public Health, 2020, 17(11):3852. doi: 10.3390/ijerph17113852.
doi: 10.3390/ijerph17113852 URL |
| [38] |
Salle JL, Lorenzo AJ, Jesus LE, et al. Surgical treatment of high urogenital sinuses using the anterior sagittal transrectal approach: a useful strategy to optimize exposure and outcomes[J]. J Urol, 2012, 187(3):1024-1031. doi: 10.1016/j.juro.2011.10.162.
doi: 10.1016/j.juro.2011.10.162 URL |
| [39] |
Fuchs J, Warmann SW, Seitz G, et al. Laparoscopically assisted vaginal pull-through for high urogenital sinus: a new surgical technique[J]. Urology, 2012, 79(5):1180-1183. doi: 10.1016/j.urology.2012.01.009.
doi: 10.1016/j.urology.2012.01.009 pmid: 22446347 |
| [1] | 许阡, 成九梅, 安圆圆. 外阴平滑肌瘤8例临床分析[J]. 国际生殖健康/计划生育杂志, 2024, 43(6): 467-470. |
| [2] | 刘思敏, 王佳丽, 张世霞, 魏佳, 杨永秀. 外阴隆突性皮肤纤维肉瘤一例[J]. 国际生殖健康/计划生育杂志, 2024, 43(6): 490-493. |
| [3] | 许阡, 成九梅. 宫颈脂肪平滑肌瘤17例临床分析[J]. 国际生殖健康/计划生育杂志, 2024, 43(5): 390-394. |
| [4] | 饶慧, 卢娇兰, 周欢, 李雄. 子宫内膜中肾样腺癌累及宫颈管间质一例[J]. 国际生殖健康/计划生育杂志, 2024, 43(5): 410-414. |
| [5] | 傅婉玉, 金莎汶, 江矞颖, 李燕青. 无创产前筛查技术在罕见常染色体三体及染色体拷贝数变异的临床效果分析[J]. 国际生殖健康/计划生育杂志, 2024, 43(4): 279-283. |
| [6] | 庄建龙, 许伟雄, 江矞颖. 全外显子组测序鉴定7q36.3微重复的胎儿多指并指畸形[J]. 国际生殖健康/计划生育杂志, 2024, 43(4): 284-288. |
| [7] | 刘芙蓉, 张钏, 周秉博, 陈雪, 田芯瑗, 马盼盼, 惠玲, 郝胜菊. 甘肃地区育龄夫妇基因扩展性携带者筛查研究[J]. 国际生殖健康/计划生育杂志, 2024, 43(4): 293-297. |
| [8] | 徐晓燕, 王笑璇. 卵巢妊娠破裂三例诊疗体会[J]. 国际生殖健康/计划生育杂志, 2024, 43(4): 309-312. |
| [9] | 何玲, 蒯丹, 张艳芳, 田文艳, 张慧英. 青春期异常子宫出血的多维评估方法[J]. 国际生殖健康/计划生育杂志, 2024, 43(4): 338-342. |
| [10] | 庄建龙, 江矞颖, 曾书红, 陈新英. FISH联合染色体核型分析明确复发性流产家系遗传病因一例[J]. 国际生殖健康/计划生育杂志, 2024, 43(3): 201-203. |
| [11] | 王晶, 王晓慧. 子宫内膜小细胞神经内分泌癌一例并文献复习[J]. 国际生殖健康/计划生育杂志, 2024, 43(3): 212-215. |
| [12] | 李彦林, 何银芳. 产科抗磷脂综合征诊治现状[J]. 国际生殖健康/计划生育杂志, 2024, 43(3): 254-259. |
| [13] | 程诗语, 石洁, 李艳丽, 高晗. 外阴硬化性苔藓的临床研究进展[J]. 国际生殖健康/计划生育杂志, 2024, 43(3): 260-264. |
| [14] | 周佳妍, 董海伟, 史云芳. 胎儿脑积水诊断Walker-Warburg综合征一例[J]. 国际生殖健康/计划生育杂志, 2024, 43(2): 108-110. |
| [15] | 王敏, 许飞雪. 梅干腹综合征一例并文献复习[J]. 国际生殖健康/计划生育杂志, 2024, 43(2): 111-114. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||